For a large majority of the population, it’s inevitable: Our eye doctor is going to tell us, if we’re over 50, that we have cataracts. But as fear-conjuring as the term “cataracts” always sounds or looks, it should be comforting to know that modern cataract surgery can usually restore lost vision – and can often reduce one’s dependence on eyeglasses, as well.
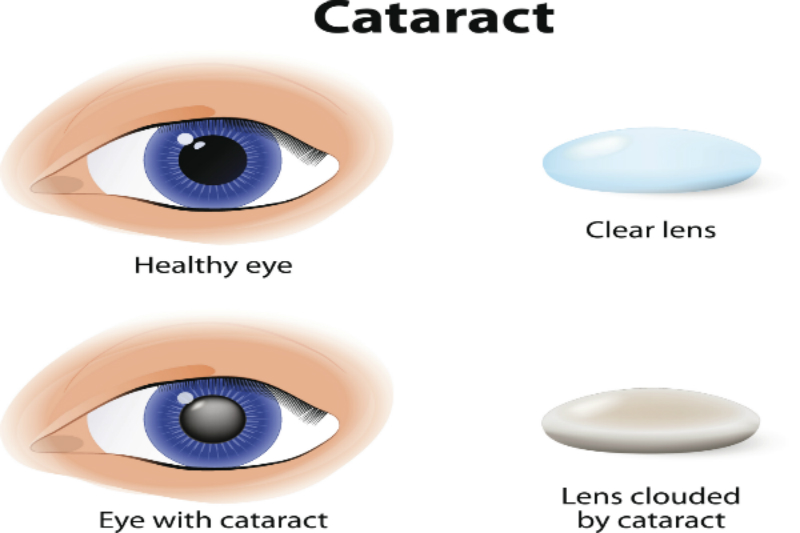
Defined as a clouding of the lens inside the eye causing loss of vision that cannot be corrected with contact lenses, glasses or corneal refractive surgery like LASIK, cataracts are associated with the aging process and remains a condition common among older people.
Rowan Eye Center Not-So-Fun Fact: According to the National Eye Institute (NEI), 68.3-percent of Americans 80 and older reported cataracts in 2010. Additionally, more than three million cataract surgical procedures are performed in the U.S. every year, with the vast majority of these yielding “excellent visual outcomes.”
The Basics
When surgery for cataracts is performed, the lens inside the eye that has become cloudy is removed and replaced with an artificial lens – referred to as an intraocular lens, or IOL – so clear vision can be restored. The procedure is generally performed on an outpatient basis, and does not require an overnight stay in a hospital or other medical care facility.
Most cataract procedures done today involve the use of a high-frequency ultrasound device that breaks up the lens that’s cloudy into small pieces, which are then gently removed from the eye via suction. This implementation, known as phacoemulsification, or “phaco,” can be performed with smaller incisions compared to cataract removal surgical techniques of the past, thus promoting quicker healing and reduction of complications such as retinal detachment.
Once all remnants of the cloudy lens have been removed from the eye, a cataract surgeon inserts a clear intraocular lens and positions it securely behind the iris and pupil – in the same position the eye’s natural lens occupied. In special unique cases, an IOL might be placed in front of the iris and pupil, though this is not as commonly seen.
The surgeon then completes the removal of the cataract and IOL implementation procedure by closing the incision in the eye (a stich may or may not be required), and a protective shield is placed over the eye to keep it safe in the early stages of recovery.
The Laser Factor
Recently, Rowan Eye Center has been studying the advantages of femtosecond lasers – similar to the lasers used to create the corneal flap in all-laser LASIK procedures – being that they’ve been approved by the FDA for use in cataract surgeries performed in the U.S. According to our research, these lasers have garnered approval for the following stages in surgery for cataracts, reducing the need for blades and other hand-held devices:
1. Creating corneal incisions to allow the surgeon access to the lens
2. Removing the anterior capsule of the lens
3. Fragmenting the cataract so less phaco energy is required to break it up and remove it
4. Creating peripheral corneal incisions to reduce astigmatism (as needed)
But here are some tidbits we’d like to share about cataract laser surgery: This procedure (also more accurately referred to as cataract laser-assisted surgery) is somewhat new and significantly increases cost, and while studies have suggested that lasers can improve accuracy during certain stages of such surgery, they may not necessarily improve factors such as recovery time, safety and visual outcomes in every single case.
For the latest information about cataract laser surgery, patients can call our offices or inquire during a preoperative eye exam and surgery consultation.
Preparing for Surgery and Choosing an IOL
An optometrist and/or ophthalmologist, prior to performing surgery on cataracts, will perform a comprehensive eye exam to check overall eye health, determine if there are any reasons a patient shouldn’t have the surgery and identify any risk factors involved. What’s more, a refraction will be performed to accurately assess the amount of farsightedness, nearsightedness and/or astigmatism a patient exudes prior to surgery. Additional measurements of the eyes are taken to determine the curvature of the cornea and length of the actual eye.
Why are these eye health measurements essential? They help the cataract surgeon select the intraocular lens’ proper power and provide the patient the best vision possible after the surgery.
Today, there are many types of IOLs to choose from for surgery on cataracts depending on specific needs; in addition to IOLs that correct nearsightedness and farsightedness, there are now “toric IOLs” that address astigmatism, as well. For most patients that don’t mind wearing glasses after surgery, a monofocal lens implant is typically used, and often times only part-time use of reading glasses is required after surgery featuring monofocal IOLs. In the case that prescription eyeglasses are required (what often occurs when only one eye needs surgery), an eye doctor usually prescribes new glasses approximately one month after surgery.
The Recovery Stage
Cataract surgeries without complications typically last only about 15 minutes, but patients can expect to be at the surgical center for 90 minutes or longer because extra time is required to prep (dilating the pupil, administering preoperative medication, etc.) and for a brief post-op evaluation to go over instructions about the surgery before the patient leaves.
It is a must that a patient bring someone who can drive him or her home following the surgery, and prescribed medicated eye drops are typically administered to be used several times each day for a few weeks.
A representative of Rowan Eye Center can provide additional instructions and recommendations when it comes to cataract surgery recovery, depending on specific needs and the outcome of a procedure. Call our offices today to schedule an appointment if you’re experiencing any of the cataract symptoms we’ve mentioned.